According to studies, wound management makes up around four per cent of the total NHS budget, coming in at £8.3bn per year. Of that figure, diabetes related foot ulcers make up 10-12 per cent, accounting for close to £1bn of NHS spending per annum. Better monitoring of these wounds has the potential to save money, time and reduce the 7,000 amputations relating to diabetic foot ulcers that take place in England each year.
Related content
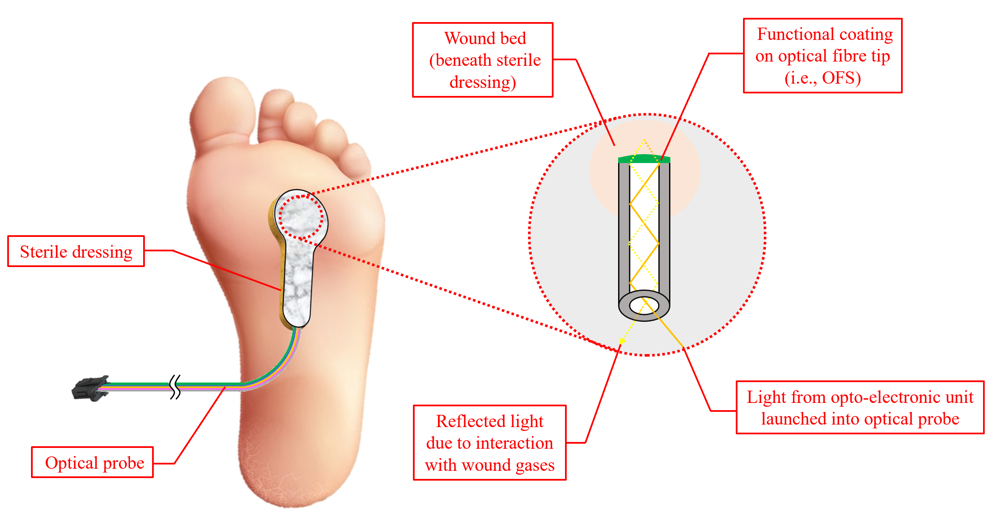
Backed by a grant of nearly £1m from the Medical Research Council, the project team is developing a dressing embedded with optical fibre sensors that can assess whether affected tissue is healing or infected. A trial of the smart wound system will see ten diabetic patients with foot ulcers have the dressings applied and monitored on a fortnightly basis for a total of eight weeks per patient. During appointments, the wounds will be assessed, with smart dressings applied for up to one hour under observation while measurements are taken.
“Currently, regular wound redressing is the only way to visually assess healing rates, which can be detrimental as it can encourage infection and disrupt progress – not to mention the resulting economic burden on NHS resources,” said Professor Steve Morgan, co-director of the Centre for Healthcare Technologies and Professor of Biomedical Engineering at Nottingham University.
“Our smart wound dressing addresses this through the incorporation of optical fibre sensors, which can remotely monitor multiple factors associated with wound management, such as temperature, humidity and gases associated with healing and infection. This has the potential to indicate the optimum time for changing the dressing and could alert clinicians about whether an intervention is required for an infected or slow-healing wound. If successful, the impact would be a reduction in the number of healthcare appointments along with improved patient care.”
According to the researchers, the dressings will cost more than existing treatments up front. However, the team hopes to prove that this will be offset by fewer dressing changes or clinical visits as well as better patient outcomes.
“Even a ten per cent reduction in costs associated with visits and appointments would provide significant annual savings of approximately £300m for the NHS, but this is just one of the elements we’re looking to achieve through this research,” said Dr David Gomez, Assistant Professor in Optical Fibre Sensing for Healthcare and Medical Devices from the Faculty of Engineering, University of Nottingham.
“If we’re able to generate a better understanding of ulcer healing and monitoring, we should be able to drastically reduce the number of amputations for future patients, because intervention when a wound gets infected will be quicker and more accurate, and usher in a new approach to chronic wound care.”
The project team includes clinicians at University Hospitals of Derby and Burton NHS Foundation Trust, Nottingham-based smart textiles company Footfalls and Heartbeats, and the Clinical Engineering Department at Nottingham University Hospitals NHS Trust.











McMurtry Spéirling defies gravity using fan downforce
What a fun demonstration. I wonder if they were brave enough to be in the car when it was first turned over. Racing fan cars would be an interesting...