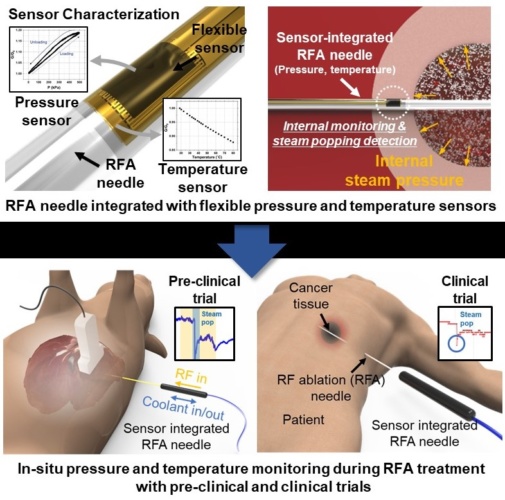
The sensors, integrated onto a 1.5mm diameter needle tip, are said to have proven their efficacy during clinical tests and expect to provide a new opportunity for safer and more effective medical practices.
Radiofrequency ablation (RFA) is a minimally invasive surgery technique for removing tumours and treating cardiovascular disease. During a procedure, an unintended audible ‘steam pop’ can occur due to the increased internal steam pressure in the area being ablated. According to the team at KAIST (Korea Advanced Institute of Science and Technology) this phenomenon has been cited as a cause of various negative thermal and mechanical effects on neighbouring tissue.
MORE FROM MEDICAL & HEALTHCARE
KAIST’s Professor Inkyu Park said that his team’s integrated sensors reliably detected the occurrence of steam pop. The sensors also monitor rapidly spreading hot steam in tissue. It is expected that the diverse properties of tissue undergoing RFA could be checked by utilising the physical sensors integrated on the needle.
“We believe that the integrated sensors can provide useful information about a variety of medical procedures and accompanying environmental changes in the human body, and help develop more effective and safer surgical procedures,” Professor Park said in a statement.
Professor Park’s team built a thin film type pressure and temperature sensor stack with a thickness of less than 10μm using a microfabrication process. For the pressure sensor, the team used contact resistance changes between metal electrodes and a carbon nanotube coated polymeric membrane. The entire sensor array was insulated with medical tubes to minimise any exposure of the sensor materials to external tissue and maximise its biocompatibility.
During the clinical trial, the research team found that the accumulated hot steam is suddenly released during steam pops and this hot air spreads to neighbouring tissue, which accelerates the ablation process. Furthermore, using in-situ ultrasound imaging and computational simulations, the research team could confirm the non-uniform temperature distribution around the RFA needle can be one of the primary reasons for the steam popping.
Professor Park added that various physical and chemical sensors for different targets can be added to create other medical devices and industrial tools.
“This result will expand the usability and applicability of current flexible sensor technologies. We are also trying to integrate this sensor onto a 0.3mm diameter needle for in-vivo diagnosis applications and expect that this approach can be applied to other medical treatments as well as the industrial field,” said Professor Park.
The team’s findings have been published in Advanced Science.





Poll: Should the UK’s railways be renationalised?
Rail passenger numbers declined from 1.27 million in 1946 to 735,000 in 1994 a fall of 42% over 49 years. In 2019 the last pre-Covid year the number...